The Dangers of MSG
Monosodium Glutamate, a food ingredient, was invented in 1908 in Japan, by Kikunae Ikeda. A year later, with a partner, he formed a company, Ajinomoto, to produce the product. The food additive did not appear in the United States to any degree until the late 1940s, following the Second World War. During the war, it had been noted that Japanese soldiers’ rations tasted better than the rations used by our soldiers. The difference was believed to be “monosodium glutamate.” Today, “monosodium glutamate” or its reactive component, “processed free glutamic acid,” is found in almost all of the processed foods that are manufactured in the United States.
ADVERSE EFFECTS OF MSG
In 1957, Lucas and Newhouse found that normal neonatal mice suffered acute degenerative lesions in the inner retina when “monosodium glutamate” was administered by feeding tube.1 In 1968, during a replication of this study at Washington University Medical School, St., Louis, Missouri, Dr. John W. Olney2 noted that, some of the mice had become grotesquely obese. He decided to sacrifice some of the mice to confirm his belief that lesions would be found in the hypothalamus region of the brain. Not only was his suspicion confirmed, but further testing indicated that there were also other neuroendocrine effects from the “monosodium glutamate.”
His findings were published in 1969.2 Dr. Olney, a National Academy of Science scientist who is credited for the voluntary removal of MSG from baby food in the 1970s, continues to publish research3-5 on the toxicity of glutamic acid, often using “monosodium glutamate.”In 1968, the New England Journal of Medicine published a Letter to the Editor in which Ho Man Kwok, MD, asked for help in determining why he and his friends suffered reactions shortly after eating in some Chinese restaurants, though he never experienced such reactions when he lived in China.
The journal titled the letter “Chinese Restaurant Syndrome,”6 and researchers from around the country wrote the journal to suggest that Dr. Kwok and his friends’ problem was intolerance to MSG. One letter indicated that 30% of the population reacted to MSG. In 1969, concerned with the bad reports regarding “monosodium glutamate,” the glutamate industry formed a nonprofit organization to defend the safety of MSG, the International Glutamate Technical Committee. Later, in 1977, they increased their efforts with the development of a nonprofit subsidiary, The Glutamate Association, primarily operating as a public relations arm of the glutamate industry. In about 1990, the glutamate industry turned to the International Food Information Council (IFIC), another nonprofit industry-funded organization, to be their spokesman and to promote the safety of MSG along with the other products that they represent.
MSG IS TOXIC TO HUMANS!
The literature is clear in demonstrating that MSG is toxic to humans and that over 25% of the population suffer adverse reactions from MSG7-36. In the opinion of this writer, the subject is only controversial because of the input of the three organizations mentioned above and because of research they have funded to discredit findings of others and to tell the story that the glutamate industry wants told, research that is flawed to the point of being worthless. “Monosodium glutamate” is approximately 78% processed free glutamic acid and 22% sodium (salt) and moisture, with about 1% contaminants.
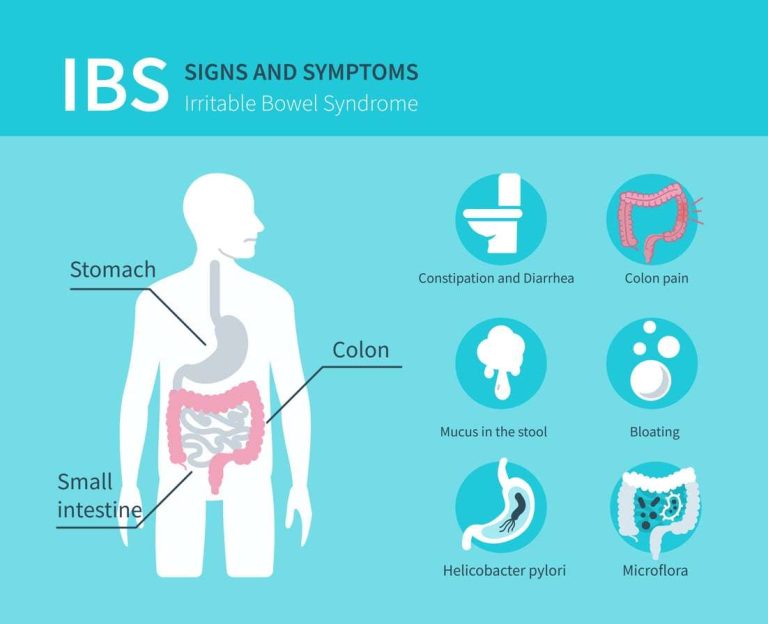
It is the processed free glutamic acid that causes people to suffer adverse reactions, and, unfortunately, there are over 40 food ingredients other than “monosodium glutamate” that contain processed free glutamic acid in varying amounts.37 Consequently, consumers refer to all processed free glutamic acid as MSG, regardless of the name of the ingredient. People differ in their tolerances to MSG, but typically always suffer similar reactions each time they ingest amounts of MSG that exceed their tolerances for the substance. Reactions experienced vary dramatically, as if MSG finds the weak link in the body.38
Typically, people will suffer reactions at approximately the same time each time they ingest amounts of MSG that exceed their tolerance levels. However, that time lapse can vary among people from immediately following ingestion of MSG up to 48 hours following ingestion. Use of alcohol or exercise prior to, during or following an MSG-containing meal will exacerbate an MSG reaction in many people. MSG-sensitive people will typically suffer similar reactions to aspartame. Neuroscientists believe that the young and the elderly are most at risk from MSG. In the young, the blood-brain barrier is not fully developed, exposing the brain to increased levels of MSG that has entered the bloodstream. The elderly are at increased risk because the blood-brain barrier can be damaged by aging, by disease processes, or by injury, including hypertension, diabetes, hypoglycemia, and stroke.
Throughout life, the blood-brain barrier is “leaky” at best. MSG has now been implicated in a number of the neurodegenerative diseases, including ALS (Lou Gehrig’s disease), Parkinson’s disease, Alzheimer’s disease, multiple sclerosis and Huntington’s disease39. In general, the natural glutamic acid found in food does not cause problems, but the synthetic free glutamic acid formed during industrial processing is a toxin. In addition, when MSG is formed using hydrochloric acid the final product includes carcinogens.40
MSG IN INFANT FORMULA: BAD FOR YOUR BABY!
A Canadian Study41 conducted, leaves no room for doubt that ingredients that contain processed free glutamic acid (MSG) and free aspartic acid — known neurotoxins— are used in baby formula. The fact that neurotoxins are present in baby formula is of particular concern since the blood brain barrier is not fully developed in infants, allowing neurotoxins to be more accessible to the brain than is the case in healthy adults. In studies using experimental animals, neuroscientists have found that glutamic acid and aspartic acid load on the same receptors in the brain, cause identical brain lesions and neuroendocrine disorders, and act in an additive fashion.
You will note that the level of neurotoxins found in the hypoallergenic formula was far greater than the level of neurotoxins found in the other formulas. In reviewing the literature on hypoallergenic formulas, we have found short-term studies that concluded that hypoallergenic formulas are safe because babies tolerated them and gained weight. However, we have not seen any long-term studies on the safety of hypoallergenic formulas. We believe that well designed long term studies would demonstrate that infants raised on hypoallergenic formulas, as compared to infants who are breastfed or fed on non-hypoallergenic formulas, will exhibit more learning disabilities at school age, and/or more endocrine disorders, such as obesity and reproductive disorders, later in life. Long-term studies on the effects of hypoallergenic formulas need to be done42.
To put these figures in perspective, consider that in an FDA-sponsored study dated July, 1992 entitled “Safety of Amino Acids Used in Dietary Supplements,” the Federation of American Societies for Experimental Biology concluded, in part, that “…it is prudent to avoid the use of dietary supplements of L-glutamic acid by pregnant women, infants, and children. . . and. . . by women of childbearing age and individuals with affective disorders.” (MSG is called glutamic acid or L-glutamic acid when used in supplements.)43 During the 1960s, the food ingredient “monosodium glutamate” was routinely added to baby foods.
The industry “voluntarily” ceased the practice after Congressional hearings in which concerned researchers warned of serious adverse effects. However, for some years following the elimination of “monosodium glutamate,” hydrolyzed proteins were used in place of “monosodium glutamate.” Hydrolyzed proteins always contain MSG. Many consumers now know to avoid baby foods with hydrolyzed proteins. Yet how many parents realize that MSG lurks in every bottle of formula given to their infants? Babies on hypoallergenic formulas receive about 1 gram of total neurotoxins per day, a level at which many MSG-sensitive individuals experience adverse reactions.
Our advice to you is to do your best to eliminate MSG from your diet. You will feel better. That means avoiding all processed foods. Our advice to investigators of school violence is to investigate the effects of excitotoxins in children’s diets. There are high levels of MSG in soy products and seasoning mixes used in school lunch programs, fast foods and snack foods. Written by Dr. George J Georgiou and Barbara Karafokas DaVinci Natural Health Centre, Larnaca, Cyprus drgeorge@avacom.net www.naturaltherapycenter.com
REFERENCES
1. Lucas, D.R., and Newhouse, J.P. (1957) The toxic effect of sodium L-glutamate on the inner layers of the retina. AMA Arch Ophthal 58: 193-201.
2. Olney, J.W. (1969). Brain lesions, obesity, and other disturbances in mice treated with monosodium glutamate. Science 164: 719-721.
3. Olney, J.W. (1993, April). Prepared statement for the public meeting (April 1993) pertaining to adverse reactions to monosodium glutamate (MSG). Presented at a public meeting conducted by the Federation of American Societies for Experimental Biology (FASEB), Bethesda, MD.
4. Olney, J.W. and Price M.T. (1978). Excitotoxic amino acids as neuroendocrine probes. In E.G. McGeer, J.W. Olney, and P.L. McGeer (Eds.), Kainic Acid as a Tool in Neurobiology. New York: Raven. 5. Olney, J.W. and Price, M.T. (1980). Neuroendocrine interactions of excitatory and inhibitory amino acids. Brain Research Bulletin
5: Suppl 2, 361-368.
6. Chinese restaurant syndrome. (1990, January). Mayo Clinic Nutrition Letter.
7. Altman, D.R., Fitzgerald, T. & Chiaramonte, L.T. (1994). Double-blind placebo-controlled challenge (DBPCC) of persons reporting adverse reactions to monosodium glutamate (MSG). J. Allergy and Clinical Immunology Abstracts 93:303 (Abstract 844).
8. Garattini, S. (1979). Evaluation of the neurotoxic effects of glutamic acid. In R.J. Wurtman, & J.J. Wurtman (Eds.), Nutrition and the brain. New York: Raven Press.
9. Geha, R., Beiser, A., Ren, C., Patterson, R., Greenberger, P., Grammer, L.C., Ditto, A.M., Harris, K.E., Shaughnessy, M.A., Yarnold, P., Corren, J., Saxon, A. (1998). Multicenter multiphase double blind placebo controlled study to evaluate alleged reactions to monosodium glutamate (MSG). J. Allergy Clin Immunol Abstracts 101:S243 (Abstract 106).
10. Germano, P., Cohen, S.G., Hahn, B., and Metcalfe, D.D. (1991). An evaluation of clinical reactions to monosodium glutamate (MSG) in asthmatics using a blinded, placebo-controlled challenge. J Allergy Clin Immunol Abstracts 87:177 (Abstract 155).
11. Giacometti, T. (1979). Free and bound glutamate in natural products. In L.J. Filer, Jr., S. Garattini, M.R. Kare, W.A. Reynolds, and R.J. Wurtman, (Eds), Glutamic acid: advances in biochemistry and physiology. New York: Raven.
12. Anantharaman, K. (1979). In utero and dietary administration of monosodium L-glutamate to mice: reproductive performance and development in a multigeneration study. In L.J. Filer, Jr., S. Garattini, M.R. Kare, W.A. Reynolds, and R.J. Wurtman, (Eds), Glutamic acid: advances in biochemistry and physiology. New York: Raven.
13. Auer, R.N. (1991). Excitotoxic mechanisms, and age-related susceptibility to brain damage in ischemia, hypoglycemia and toxic mussel poisoning. NeuroToxicology 12:541-546.
14. Bunyan, J., Murrell, E.A., and Shah, P.P. (1976). The induction of obesity in rodents by means of monosodium glutamate. Br J Nutr 35: 25-29.
15. Ebert, A.G. (1970). Chronic toxicity and teratology studies of monosodium L-glutamate and related compounds. Toxicol Appl Pharmacol 17: 274.
16. Federation of American Societies for Experimental Biology (FASEB) (1995). Analysis of adverse reactions to monosodium glutamate (MSG). Bethesda, MD: Life Sciences Research Office, FASEB.
17 Fernstrom, J.D., Cameron, J.L., Fernstrom, M.H., McConaha, C., Weltzin, T.E., and Kaye, W.H. (1996). Short-term neuroendocrine effects of a large, oral dose of monosodium glutamate in fasting male subjects. J Clin Endocrinol Metab 81: 184-191.
18. Filer, L. J. (1993). Public Forum: analysis of adverse reactions to monosodium glutamate. Paper presented at open meeting of the Federation of American Societies for Experimental Biology, April 1993.
19. Kenney, R.A. (1979). Placebo-controlled studies of human reaction to oral monosodium L-glutamate. In L.J. Filer, Jr., S. Garattini, M.R. Kare, W.A. Reynolds, and R.J. Wurtman, (Eds), Glutamic acid: advances in biochemistry and physiology. New York: Raven.
20. Kenney, R.A., and Tidball, C.S. (1972). Human susceptibility to oral monosodium L-glutamate. A J Clin Nutr 25:140-146.
21. Nemeroff, C.B. (1981). Monosodium glutamate-induced neurotoxicity: review of the literature and call for further research. In S.A. Miller (Ed.), Nutrition & behavior. Philadelphia: Franklin Institute Press.
22. Newman, A.J., Heywood, R., Palmer, A.K., Barry, D.H., Edwards, F.P., and Worden, A.N. (1973). The administration of monosodium L-glutamate to neonatal and pregnant rhesus monkeys. Toxicology 1: 197-204.
23. Owen, G., Cherry, C.P., Prentice, D.E., and Worden, A.N. (1978). The feeding of diets containing up to 4% monosodium glutamate to rats for 2 years. Toxicol Lett 1: 221-226.
24. Pulce, C., Vial, T., Verdier, F., et al. (1992). The Chinese restaurant syndrome: a reappraisal of monosodium glutamate’s causative role. Adverse Drug Reaction Toxicology Review pp.19-39.
25. Reif-Lehrer, L. (1977). A questionnaire study of the prevalence of Chinese restaurant syndrome. Fed Proc 36:1617-1623.
26. Reynolds, W.A., Butler, V., Lemkey-Johnston, N. (1976). Hypothalamic morphology following ingestion of aspartame or MSG in the neonatal rodent and primate: a preliminary report. J Toxicol environmental Health 2: 471-480.
27. Reynolds, W.A., Filer, L. J., and Stegink, L.D. (1991). Letter to Dr. Kenneth G. Fisher, LSRO, FASEB. May 31, 1991.
28. Reynolds, W.A., Lemkey-Johnston, N., Filer, L.J. Jr., and Pitkin, R.M. (1971). Monosodium glutamate: absence of hypothalamic lesions after ingestion by newborn primates. Science 172: 1342-1344.
29. Samuels, A. (1995). Monosodium L-glutamate: a double-blind study and review. Letter to the editor. Food and Chemical Toxicology. 33: 69-78.
30. Schaumburg, H.H., Byck, R., Gerstl, R. and Mashman, J.H. (1969) Monosodium L-glutamate: its pharmacology and role in the Chinese restaurant syndrome. Science 163: 826-828.
31. Scopp, A.L.(1991). MSG and hydrolyzed vegetable protein induced headache: review and case studies. Headache 31:107-110.
32. Takasaki, Y., Matsuzawa, Y., Iwata, S., O’Hara, Y., Yonetani, S., and Ichimura, M. (1979a). Toxicological studies of monosodium L-glutamate in rodents: relationship between routes of administration and neurotoxicity. In L.J. Filer, Jr., S. Garattini, M.R. Kare, W.A. Reynolds, and R.J. Wurtman, (Eds), Glutamic acid: advances in biochemistry and physiology. New York: Raven.
33 Takasaki, Y., Sekine, S., Matsuzawa, Y., Iwata, S., and Sasaoka, M. (1979b). Effects of parenteral and oral administration of monosodium L-glutamate (MSG) on somatic growth in rats. Toxicol Lett 4: 327-343.
34. Taliferro, P.J. (1995). Monosodium glutamate and the Chinese restaurant syndrome: a review of food additive safety. J. Environmental Health 57: 8-12.
35. Tarasoff, L and Kelly, M.F. (1993). Monosodium L-glutamate: a double-blind study and review. Food Chem Toxic 31:1019-1035.
36. Yang, W.H., Drouin, M.A., Herbert, M., and Mao, Y. (1997). The monosodium glutamate symptom complex: Assessment in a double-blind, placebo-controlled, randomized study. J Allergy Clin Immunol 99: 757-762.
37. Daniels, D.H., Joe, F.L. and Diachenko, G.W. (1995). Determination of free glutamic acid in a variety of foods by high-performance liquid chromatography. Food Additives and Contaminants 12:21-29.
38. Blaylock, R.L. (1994). Excitotoxins: the taste that kills. Santa Fe: Health Press.
39. Taylor, S.L. (1993, April). Possible adverse reactions to hydrolyzed vegetable protein. Paper submitted to the Federation of American Societies for Experimental Biology review panel.
40. Goldschmiedt, M., Redfern, J.S., and Feldman, M. (1990). Food coloring and monosodium glutamate: effects on the cephalic phase of gastric acid secretion and gastrin release in humans. Am J Clin Nutr 51: 794-797.
41. Appreciation to Baby Love Products Inc. of Camrose, Alberta, Canada (www.kidalog.com)
42. Taken from Jack Samuels and his wife, Adrienne Samuels, PhD, who are founders of Truth in Labeling, a nonprofit organization dedicated to accurate labelling of MSG and the removal of MSG from use in agriculture. For further information, see their website at www.truthinlabeling.org.
43. Leibovitz, B. Safety of amino acids used as dietary supplements. Am. J. Clinical Nutrition, Vol. 57, Issue 6, b -946, June 1, 1993
Read other interesting articles: