Gluten Intolerance (Celiac Disease)
INTRODUCTION
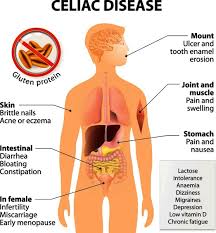
Celiac disease, also known as gluten intolerance, is a genetic disorder that affects 1 in 133 (11). Americans. Symptoms of celiac disease can range from the classic features, such as diarrhea, weight loss, and malnutrition, to latent symptoms such as isolated nutrient deficiencies but no gastrointestinal symptoms. The disease mostly affects people of European descent, and may occur more rarely in black and Asian populations (13). Those affected suffer damage to the villi (shortening and villous flattening) in the lamina propria and crypt regions of their intestines when they eat specific food-grain antigens (toxic amino acid sequences) that are found in wheat, rye, and barley (13). Oats have traditionally been considered to be toxic to celiacs, but recent scientific studies have shown otherwise. This research is ongoing, however, and it may be too early to draw solid conclusions.
Because of the broad range of symptoms celiac disease presents, it can be difficult to diagnose. The symptoms can range from “mild weakness, bone pain, and aphthous stomatitis to chronic diarrhea, abdominal bloating, and progressive weight loss (13).” If a person with the disorder continues to eat gluten, studies have shown that he or she will increase their chances of gastrointestinal cancer by a factor of 40 to 100 times that of the normal population (14). Further, “gastrointestinal carcinoma or lymphoma develops in up to 15 percent of patients with untreated or refractory celiac disease (13).” It is therefore imperative that the disease is quickly and properly diagnosed so it can be treated as soon as possible.
Based on the figure mentioned above we can extrapolate the total number of people in the United States with celiac disease: 2,131,019 (based on the total population: 283,425,607 (15). It is very important that doctors understand just how many people have this disease so that routine testing for it is done to bring the diagnosis rate in line with the disease’s epidemiology. Testing is fairly simple and involves screening the patient’s blood for antigliadin (AGA) and endomysium antibodies (EmA), and/or doing a biopsy on the areas of the intestines mentioned above, which is still the standard for a formal diagnosis.
The only acceptable treatment for celiac disease is strict adherence to a 100% gluten-free diet for life. An adherence to a gluten-free diet can prevent almost all complications caused by the disease (13). A gluten-free diet means avoiding all products that contain wheat, rye and barley, or any of their derivatives. This is a difficult task as there are many hidden sources of gluten found in the ingredients of many processed foods.
In the Lancet recently (1) a consistent cohort of patients affected by drug-resistant epilepsy with cerebral calcifications where all cured when they were placed on a gluten-free diet. All had an atrophic jejunal mucosa, which recovered on a gluten free diet. Gluten intolerance is now a recognized cause of brain calcifications and epilepsy, of dementia, of psychiatric disturbances: many researchers believe that, in genetically predisposed subjects, gluten is not healthy for the brain function (2).
On the other end of the spectrum, we know that there are many gluten intolerant people that do not manifest any complaints even though they have a flat intestinal mucosa (3). It is considered that about 0.3 – 1 percent of the population are gluten intolerant and react with a wide spectrum of symptoms from no apparent reaction to severe life-threatening diseases.
WHAT IS GLUTEN INTOLERANCE
Celiac disease (CD) also referred to as gluten sensitive enteropathy (GSE), gluten intolerance, or celiac sprue. It is considered to be the most under-diagnosed common disease today, affecting 1in every 170 to 250 people in the USA. It is a chronic, inherited disease, and if untreated can ultimately lead to malnutrition. Gluten intolerance is the result of an autoimmune system response to the ingestion of gluten (from wheat, rye, and barley) that damages the small intestine. Nutrients then quickly passed through the small intestine, rather than being absorbed. To develop celiac disease (CD) three (3) things must be present: 1) you must inherit the gene, 2) consume gluten, and 3) have the gene triggered. Common triggers include stress, trauma (surgeries, pregnancy, etc.), and viral infections. Approximately 10% of first-degree relatives could have CD triggered in their lifetime. The disease is permanent and damage to the small intestine will occur every time you consume gluten, regardless if symptoms are present.
This intolerance is strongly linked to specific genetic markers which have evolved over thousands of years, along with environmental and dietary changes that have occurred over the last century or so.
TREATMENT
Dietitians developed the following dietary guidelines, for the Gluten Intolerance Group® and Celiac Disease Foundation. These are in agreement with the Gluten Free Diet guidelines published by the American Dietetic Association, October 2000. The American Dietetic Association Guidelines were written through a cooperative effort of dietitian experts in celiac disease in Canada and the United States.
The following grains & starches are allowed:
- · Buckwheat
- · Rice
- · Corn
- · Potato
- · Tapioca
- · Bean
- · Sorghum
- · Soy
- · Arrowroot
- · Amaranth
- · Quinoa
- · Millet
- · Tef
- · Nut Flours
The following grains contain gluten and are not allowed:
- · Wheat (durum, semolina)
- · Rye
- · Barley
- · Spelt
- · Triticale
- · Kamut
- · Farina
The following ingredients are questionable and should not be consumed unless you can verify they do not contain or are derived from prohibited grains:
- · Brown rice syrup (frequently made with barley)
- · Caramel color
- · Dextrin (usually corn, but may be derived from wheat)
- · Flour or cereal products
- · Hydrolyzed vegetable protein (HVP), vegetable protein, hydrolyzed plant protein (HPP), or textured vegetable protein (TVP)
- ·
- · Modified food starch or modified starch
- · Mono- & di-glycerides (in dry products only)
- · Natural and artificial flavors
- · Soy sauce or soy sauce solids (many soy sauces contain wheat)
Additional components frequently overlooked that often contain gluten:
- · Breading
- · Broth
- · Coating mixes
- · Communion Wafers
- · Croutons
- · Imitation bacon
- · Imitation seafood
- · Marinades
- · Pastas
- · Processed Meats
- · Roux
- · Sauces
- · Self-basting poultry
- · Soup base
- · Stuffing
- · Thickeners
Can I Use Oats?
Based on numerous studies in the last several years, involving children and adults, using pure oats and store-shelf oats, around the world; research shows that oats do not appear to be harmful to persons with gluten intolerance in moderation. Recent discovery of the specific reactive peptide in gluten intolerance and research by Dr. Don Kasarda on the amino acid sequencing of oats vs. the now known peptide, would again clear oats as not having the reactive peptide sequence known to be problematic for gluten intolerance. Therefore oats are gluten free.
However, there is concern by the medical and research communities worldwide that the level of possible contamination of oats with gluten from unacceptable sources is too high. Therefore, GIG® is not recommending the use of oats by the celiac community.
Today, as we know and understand research on gluten intolerance, the offending cereals that must be avoided are wheat, rye, barley and their derivative cereals.
HISTORY OF CELIAC
It appears that celiac disease was reported at least a century ago. Dr. R.A. Gibbons, MD., M.R.C.P., Physician to The Grosvenor Hospital for Women and Children, Physician for the Diseases of Women and Children at the St. George’s and St. James’s Dispensary reported the following article entitled “The Coeliac Affection in Children” in the Edinburgh Med. Journ, Vol. XXXV.-NO.IV., Oct. 1889, pp. 321-330:
Case I – J.F., a boy, aged 2 years, was first seen on the 26th of April 1883
He was lying in his nurse’s lap, looking flushed, and complaining of pain over the abdomen. He had been languid and vomiting during the morning. I ascertained that the motions had been copious, frothy, and offensive. He had been latterly losing flesh. As to the previous history, I learned that the child had been brought up by hand, and there was nothing of importance to relate until last December, since which time he had been out of health, and seemed to be gradually getting worse. In that month they had sought advice, and he had caused his parents anxiety ever since, sometimes being a little better, at other times worse. On examination I found that the temperature was over 99, the pulse 108; but no definite disease could be made out. The examination of the chest yielded nothing. The abdomen was soft and doughy, but painful to the touch, and he cried out when any attempt was made to palpate. The spleen and liver were not enlarged, and I could detect no enlarged lymphatic glands. The flesh was soft and flabby. As he was having rather frequent actions of the bowels, a mixture of bismuth and compound tincture of camphor was ordered.
His diet consisted of cream, with two or three times as much water or scalded whey. For a drink at breakfast, at 11 o’clock in the morning, and at bedtime, whey made wit essence of rennet; if mixed with cream, it was to be scalded. Pounded raw meat prepared in the ordinary way, and rubbed through a sieve; of this one, two, or three tablespoonful to be taken for dinner, with a little sifted sugar or fruit jelly. A tablespoonful of mashed floury potato. Rusks, plain biscuits, or toast with fresh butter; Savory & Moore’s food made with whey, and a teaspoonful of cream added. Half a pint of asses’ milk in the morning, and the same quantity- in the evening. One or two teaspoonfuls of raw meat in the after part of the day. The following day I carefully examined some motion microscopically, and could detect no pus and nothing extraordinary.
Family History: – The mother was a healthy woman. She had had no miscarriage.
She had no history of any important disease. There was no trace of tubercle on her side. Her mother suffered occasionally from gout. The child’s father appeared a healthy man; he occasionally passed free uric acid, and had symptoms rather like those of renal calculus. There was no history of syphilis obtainable, and no reason to suspect it. There were two other children, a boy and girl, older than this patient. The girl had suffered from suppuration of the submaxillary glands.
The child improved considerably until 5th July, when he had an attack of watery- diarrhea, which prostrated him. The motions were extremely offensive. Dr. Gee saw him with me, and suggested, instead of the compound kino powder, which he was taking, that he should have minute doses of mercury and chalk every two hours; forty-eight hours later the diarrhea had stopped. Without going further into detail, it may be stated that this attack nearly proved fatal. He, however, gradually recovered, the first favorable sign being that the motion contained some solid material. There was no change in the diet, except that the meat was omitted and Brand’s essence substituted.
The following month left London for the seaside. He occasionally had attacks of diarrhea there. Six months afterwards I again saw him, when he seemed in excellent spirits, looked fat, and, although flabby, ran about and played with the other children with apparent enjoyment.
This boy died of acute purpura haemorrhagica, the details of which illness I have already published in the Medical Times and Gazette for 1885.
STANFORD RESEARCHERS FIND CAUSE AND POSSIBLE CURE FOR GLUTEN
A team of investigators led by Stanford University researchers have discovered the cause and a potential treatment for celiac sprue, an autoimmune disease that leads to an inability to digest gluten, a major protein in wheat, rye and barley products. The disease is estimated to afflict as many as 1 in 200 Americans.
In the Sept. 27 issue of Science, researchers identify a fragment of gluten called gliadin as the celiac culprit. They showed that this fragment is resistant to digestion and is responsible for the intestine-damaging inflammatory response experienced by celiac patients. They also report the use of a dietary enzyme made by a bacterium that can break down the fragment into harmless bits, suggesting future treatment through dietary supplements.
“These findings are the first step to giving people with celiac disease real hope for a normal life,” said Chaitan Khosla, PhD, professor of chemistry, chemical engineering and, by courtesy, of biochemistry. Lu Shan, a graduate student in Khosla’s lab, was lead author on the paper. The team included other Stanford researchers as well as a group from the University of Oslo in Norway.
The lining of the small intestine is normally carpet-like, covered with small protrusions called villi. Celiac disease, however, results in a smooth, pipe-like intestine. The reduced surface area keeps the body from absorbing nutrients. Often diagnosed in childhood, the disease can lead to the distended stomach and stunted growth typical of starvation.
“The only effective therapy for most people is a lifelong gluten-free diet, and that’s fairly restrictive,” explained co-author Gary M. Gray, professor of medicine, emeritus. The diet is essential over the long term both to restore normal intestinal function and to reduce the risk of developing osteoporosis, lymphoma or cancer of the small intestine, he added.
In the laboratory, Shan simulated the digestive process, exposing gliadin to digestive enzymes in test tubes. She identified a protein fragment made up of 33 amino acids that was resistant to further digestion and whose structure was known to be toxic. Most proteins are broken down into small peptides of between two and six amino acids or into single amino acids. She then repeated her study in rats and again in test tubes using tissue taken by biopsy from patients undergoing unrelated medical procedures. “Even with prolonged treatment (exposure to intestinal enzymes), the peptide doesn’t lose the ability to induce the inflammatory response,” Shan said.
When they looked more closely at the fragment, Shan and her colleagues found that it was made up of even smaller fragments already known to induce human T-cells to attack the intestine. The team in Norway then measured the ability of the gliadin fragment to induce autoimmune activity. “The response by T-cells was about 10 to 20 times higher than the smaller peptides themselves,” Shan said.
Because the fragment is rich in the amino acid proline, investigators reasoned that a peptidase (an enzyme that breaks down proteins) with the ability to digest proline-rich chains might be able to break down the gliadin fragment, rendering it harmless to celiac patients. They have now shown that this is the case in test tubes and in rats. Because there are no animal models of celiac disease, testing this approach in humans is a long way off and will require further preclinical work, Khosla said. “We think that this mode of therapy – peptidase supplementation – may offer hope in treating celiac sprue eventually, and we’re going to test this hypothesis.”
REFERENCES
1. Gobbi G, Bouquet F, Greco L, Lambertini A, Tassinari CA, Ventura A, Zaniboni MG: “Coeliac Disease, epilepsy and cerebral calcifications” Lancet, 340, Nx 8817, 439-443, 1992
2. Epilepsy and other neurological disorders in Coeliac Disease. Republic of S. Marino Meeting, April 10-12 1995, G. Gobbi edt., Raven Press, in preparation.
3. Catassi C, Ratsch IM, Fabiani E, Rossini M, Bordicchia F, Candela F, Coppa GV, Giorgi PL: Coeliac Disease in the year 2000: exploring the iceberg. Lancet, 1994, 343: 200-203.
4. Furon R. Manuel de Prehistorie Generale., 1958, Payor, Paris.
5. Raven PH, Evert RF, Eichorn S Biology of plants. 4th ed. Worth Publ. Inc, New York, 1986.
6. Feldman M, Sears ER The wild gene resources of wheat. Scientific American, 1981: 98-109.
7. Lucio Giunio Moderato Columella ” Libri rei rusticae” Anni 60-65 dopo Cristo. Ed. Einaudi,1977.
8. Greco,L.: ” Malnutrizione di classe a Napoli” Inchiesta, 24, 53-63, 1976.
9. Maki M, Kallonen K, Landeaho ML, Visakorpi JK.:Changing pattern of childhood coeliac disease in Finland. Acta Paediatr Scand 1988; 77:408-412.
10. Greco L, Maki M, Di Donato F, Visakorpi JK. Epidemiology of Coeliac Disease in Europe and the Mediterranean area. A summary report on the Multicentric study by the European Society of Paediatric Gastroenterology and Nutrition. In “Common Food Intolerances 1: Epidemiology of Coeliac Disease”, Auricchio S, Visakorpi JK, editors, Karger, Basel, 1992, pp 14-24.
- Alessio Fasano, MD, et. al., Arch Intern Med. 2003;163:286-292
- Gastroenterology, April, 1996 “First Epidemiological Study of Gluten Intolerance in the United States.” By Karoly Horvath, MD, Ph.D., et. al..
- New England Journal of Medicine, May 2, 1996 — Volume 334, Number 18, “The Many Faces of Celiac Disease” by Charles H. Halsted, MD
- Goggins, et. al. “Celiac Disease and Other Nutrient Related Injuries to the Gastrointestinal Tract” The American Journal of Gastroenterology. Vol. 89, No. 8, pages S2 – S13, 1994.
- United States Census Bureau, January 7, 2001.
CELIAC DISEASE & GLUTEN INTOLERANCE INTERNET
Sites by National Support Organizations
The Celiac Disease Foundation (USA):
http://www.celiac.org/
The Celiac Sprue Association (USA):
http://www.csaceliacs.org
The Gluten Intolerance Group of North America (USA):
http://www.gluten.net/
Canadian Celiac Association:
http://www.celiac.ca/
The Coeliac Society of Ireland:
http://www.coeliac.ie/
University Sites
University of Maryland Center for Celiac Research Center for Celiac Research:
http://www.celiaccenter.org/
Read other interesting articles such as:
Feeding the Children of Tomorrow
Books on Celiac Disease
Celiac Disease: Natural Approaches for Optimal Living